This page contains relevant scientific articles, including open-access articles that may be freely downloaded without charge.
Articles authored by INR Physicians
2016-2019
-
- Tobinick, E. Immediate Resolution of Hemispatial Neglect and Central Post-Stroke Pain After PSE: Case Report. Clinical Drug Investigation: 2019 October 22, epub. FREE DOWNLOAD.
- Tobinick, E. PSE advances as a neurotherapeutic. Expert Review Neurotherapeutics: 2018:1-3. FREE DOWNLOAD.
- Tobinick E, Ignatowski, T., Spengler, R. On Overcoming Barriers to Application of Neuroinflammation Research. In: Abreu GEA, ed. Mechanisms of Neuroinflammation: InTechOpen; 2017. FREE DOWNLOAD.
- Edward Tobinick M.D. Perispinal Delivery of CNS Drugs. CNS Drugs: 2016; 30(6):469-80. FREE DOWNLOAD.
- Tobinick E, H. Rodriguez-Romanacce, R Kinssies, N Kim. PSE for Traumatic Brain Injury. Chapter 7 in New Therapeutics for Traumatic Brain Injury: Prevention of Secondary Brain Damage and Enhancement of Repair and Regeneration. Academic Press. London. 2017. Editor: Kim A Heidenreich.
Selected Open Access Articles Published in 2015 and Earlier:
- Ignatowski TA, Spengler RN, Dhandapani KM, Folkersma H, Butterworth RF, Tobinick E. PSE for post-stroke neurological and cognitive dysfunction: scientific rationale and current evidence. CNS Drugs: 2014 Aug;28(8):679-97. FREE FULL-TEXT.
- Tobinick E, Rodriguez-Romanacce H, Levine A, Ignatowski TA, Spengler RN. Immediate neurological recovery following PSE years after brain injury. Clinical Drug Investigation: 2014;34(5)361-6.
- Tobinick EL, Gross H. Rapid cognitive improvement in Alzheimer’s disease following PSE administration. J Neuroinflammation: 2008;5:2. FREE FULL-TEXT.
- Tobinick EL, Gross H. Rapid improvement in verbal fluency and aphasia following PSE in Alzheimer’s disease. BMC Neurology 2008;8:27. FREE FULL-TEXT.
- Tobinick E. PSE: a new therapeutic paradigm in neurology. Expert Review of Neurotherapeutics. 2010 Jun;10(6):985-1002. FREE FULL-TEXT.
- Tobinick EL, Chen K, Chen X. Rapid intracerebroventricular delivery of Cu-DOTA-etanrcept after peripheral administration demonstrated by PET imaging. BMC Res Notes. 2009;2:28. FREE FULL-TEXT.
- Tobinick, E., PSE produces rapid improvement in primary progressive aphasia: identification of a novel, rapidly reversible TNF-mediated pathophysiologic mechanism. Medscape J Med, 2008. 10(6): p. 135. FREE FULL-TEXT.
- Tobinick, E. The cerebrospinal venous system: anatomy, physiology, and clinical implications. MedGenMed. 2006. 8(1): p. 53. FREE FULL-TEXT.
- Tobinick EL, Britschgi-Davoodifar S. Perispinal TNF-alpha inhibition for discogenic pain. Swiss Med Wkly. 2003 Mar 22;133(11-12):170-7. FREE FULL-TEXT.
Articles authored by Independent Scientists
2016 articles:
- Excess cerebral TNF causing glutamate excitotoxicity rationalizes treatment of neurodegenerative diseases and neurogenic pain by anti-TNF agents. Clark IA, B Vissel. Journal of Neuroinflammation. 2016;13(1):236. FREE FULL-TEXT.
2014/2015 articles:
- A Neurologist’s guide to TNF biology, and to the principles behind the therapeutic removal of excess TNF in disease. Clark IA, B Vissel. Neural Plasticity, Volume 2015, Article ID 358263, http://dx.doi.org/10.1155/2015/358263. FREE FULL-TEXT.
- Studies of selective TNF inhibitors in the treatment of brain injury from stroke and trauma: a review of evidence to date. Tuttolomondo, A., R. Pecoraro, and A. Pinto, Drug Design, Development and Therapy, 2014(November). 8: p. 2221-2239. FREE FULL-TEXT.
- Action of anti-TNF-alpha drugs on the progression of Alzheimer’s disease: A case report. Carlos Henrique Ferreira Camargo, FF Justus, G Uretzlaff, MRY Blood, MD Schafranski. Dementia & Neuropsychoelogia. 9(2) April/June 2015. http://dx.doi.org/10.1590/1980-57642015DN92000015. FREE FULL-TEXT.
- Olmos G, Llado J. Tumor necrosis factor alpha: a link between neuroinflammation and excitotoxicity. Mediators Inflamm. 2014;2014:861231. FREE FULL-TEXT. Abstract includes: “Tumor necrosis factor alpha (TNF- alpha) is a pro-inflammatory cytokine that exerts both homeostatic and pathophysiological roles in the central nervous system. In pathological conditions, microglia release large amounts of TNF-alpha; this de novo production of TNF-alpha is an important component of the so-called neuroinflammatory response that is associated with several neurological disorders. …. As microglial activation and up-regulation of TNF-alpha expression is a common feature of several CNS diseases, as well as chronic opioid exposure and neuropathic pain, modulating TNF-alpha signaling may represent a valuable target for intervention.”
- Kathirvelu, B. and S.T. Carmichael, Intracerebral hemorrhage in mouse models: therapeutic interventions and functional recovery. Metab Brain Dis, 2014. FULL-TEXT. Article includes: “With direct blood extravasation into brain, secondary inflammation is a substantial feature. Drugs which reduce neuroinflammation enhance functional recovery. Lei and colleagues targeted tumor necrosis factor alpha (TNF-alpha), a cytokine that is secreted by the microglia in response to injury and acts as a prime neuroinflammatory mediator causing progressive damage. A single dose of TNF-alpha antibody, CNTO5048, via tail vein 30 min following collagenase-induced ICH in mice showed evidence of reduced neuroinflammation and improved functional deficit in the rotorod task (Lei et al. 2013). Similarly, TNF-alpha antagonist, R-7050 is tested with collagenase-induced ICH mice. Single dose of Intraperitoneal R-7050 given within 2 h of ICH showed reduced edema and blood brain barrier damage with improved neurological deficit assessed from modified 24 point scale (King et al. 2013).”
- Wang K, Liu B, Ma J. Research progress in traumatic brain penumbra. Chin Med J (Engl). 2014 May;127(10):1964-8. FREE FULL-TEXT.
- Ignatowski TA, Spengler RN, Dhandapani KM, Folkersma H, Butterworth RF, Tobinick E. PSE for post-stroke neurological and cognitive dysfunction: scientific rationale and current evidence. CNS Drugs. 2014 Aug;28(8):679-97. FREE FULL-TEXT.
- Clark IA, Vissel B. Inflammation-sleep interface in brain disease: TNF, insulin, orexin. J Neuroinflammation. 2014;11:51. FREE FULL-TEXT.
- Dacks, P.A., D.A. Bennett, and H.M. Fillit, Evidence needs to be translated, whether or not it is complete. JAMA Neurology, 2014. 71(2): p. 137-8. ARTICLE LINK. First paragraph: “Every medical decision should be based on the best available scientific evidence. This goal motivates evidence-based medicine, a movement with undisputable value that improves the rigor of research available for medical decisions. While not the original goal of evidence-based medicine, randomized clinical trials (RCTs) have not simply become the gold standard of confidence but have overshadowed and limited the use of other sources of useful information. As stated by Kaplan et al,1 “over-reliance on RCTs is similar to resting all of health care evidence on a one-legged stool.’ ”
Articles published in 2013 and earlier:
- Johnson, V.E., J.E. Stewart, F.D. Begbie, J.Q. Trojanowski, D.H. Smith, and W. Stewart, Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain, 2013. 136(Pt 1): p. 28-42. FREE FULL-TEXT.Abstract includes: “These data present striking evidence of persistent inflammation and ongoing white matter degeneration for many years after just a single traumatic brain injury in humans.”
- King MD, Alleyne CH, Jr., Dhandapani KM. TNF-alpha receptor antagonist, R-7050, improves neurological outcomes following intracerebral hemorrhage in mice. Neurosci Lett. 2013 May 10;542:92-6. FREE FULL-TEXT.
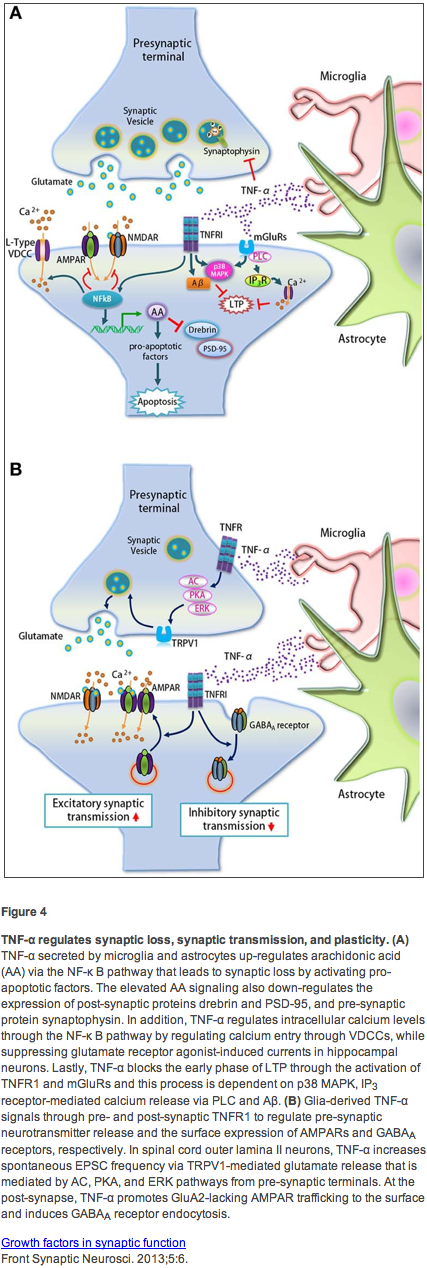
- Poon VY, Choi S, Park M. Growth factors in synaptic function. Front Synaptic Neurosci. 2013;5:6. FREE FULL-TEXT.
- Blaylock RL. Immunology primer for neurosurgeons and neurologists part 2: Innate brain immunity. Surg Neurol Int. 2013;4:118. FREE FULL-TEXT. Article includes: “Based on this central effect of TNF-alpha , Tobinick et al. demonstrated dramatic, rapid improvement among 629 consecutive stroke patients following injection of the TNF-alpha blocking drug etanrcept given perispinally (Batson’s plexus). Statistically significant improvements were seen in a wide range of neurological deficits and symptoms, including motor impairment, spasticity, sensory impairment, cognition, behavioral function, aphasia, and pain. Incredibly, they noted a strong effect even in patients having strokes as long as 10 years previously. They found similar improvements among 12 patients with traumatic brain injury.”
- Lei B, Dawson HN, Roulhac-Wilson B, Wang H, Laskowitz DT, James ML. Tumor necrosis factor alpha antagonism improves neurological recovery in murine intracerebral hemorrhage. J Neuroinflammation. 2013 Aug 20;10(1):103. FREE FULL-TEXT. Abstract includes: “Intracerebral hemorrhage (ICH) is a devastating stroke subtype characterized by a prominent neuroinflammatory response. Antagonism of pro-inflammatory cytokines by specific antibodies represents a compelling therapeutic strategy to improve neurological outcome in patients after ICH.”
- Cheong CU, Chang CP, Chao CM, Cheng BC, Yang CZ, Chio CC. Etanrcept attenuates traumatic brain injury in rats by reducing brain TNF- alpha contents and by stimulating newly formed neurogenesis. Mediators Inflamm. 2013;2013:620837. FREE FULL-TEXT.
- Kaufman EL, Carl A. Biochemistry of Back Pain. The Open Spine Journal. 2013 30 September 2013;5:12-8. FREE FULL-TEXT. Article includes: ” More recently Sainoh et al. (2013) [46] have presented a paper at the 40th ISSLS on intradiscal injection of anti TNF-alpha in a randomized study of 30 patients that echoed the finding of Tobinick et al. This study was able to look at the effects of etanrcept (as compared to bupivacaine) on low back pain patients following an injection at 1, 2 and 4 weeks using a visual analog scale and ODI. At the 4-week time point it was shown that TNF-alpha [inhibitor, etanrcept] provided patients with a statistically significant relief of pain (p<0.005) according to the ODI.”
- Iwatsuki, K., T. Arai, H. Ota, S. Kato, T. Natsume, S. Kurimoto, M. Yamamoto, and H. Hirata, Targeting anti-inflammatory treatment can ameliorate injury-induced neuropathic pain. PLoS One, 2013. 8(2): p. e57721. FREE FULL-TEXT.
- Kiene, H., H.J. Hamre, and G.S. Kienle, In support of clinical case reports: a system of causality assessment. Glob Adv Health Med, 2013. 2(2): p. 64-75. FREE FULL-TEXT.
- Clark I, Atwood C, Bowen R, Paz-Filho G, Vissel B. Tumor necrosis factor-induced cerebral insulin resistance in Alzheimer’s disease links numerous treatment rationales. Pharmacol Rev. 2012 Oct;64(4):1004-26. FREE FULL-TEXT. Article includes: ” Because the intracerebroventricular route is a precarious one, unsuited to regular administration to the same patient, a number of ways to circumvent this problem are being developed to widen the use of these highly successful biological agents to a new patient group. The earliest of these is a novel approach termed the perispinal route (Tobinick et al., 2006, 2010, 2012). Its logic depends on 1) a short period of head-down tilting to gain a gravitational advantage, 2) an awareness of anatomy of Batson’s plexus [a valveless venous system that surrounds the spinal column in continuum with the choroid plexus (Nathoo et al., 2011)], and 3) knowledge of the effect of acute hypertension on choroid plexus permeability [a 30-fold increase in albumin in CSF within 10 min of pharmacologically induced acute local hypertension (Murphy and Johanson, 1985)].”
- Folkersma H, Boellaard R, Yaqub M, Kloet RW, Windhorst AD, Lammertsma AA, et al. Widespread and prolonged increase in (R)-(11)C-PK11195 binding after traumatic brain injury. J Nucl Med. 2011 Aug;52(8):1235-9. FREE FULL-TEXT.
- Jiang H, Hampel H, Prvulovic D, Wallin A, Blennow K, Li R, et al. Elevated CSF levels of TACE activity and soluble TNF receptors in subjects with mild cognitive impairment and patients with Alzheimer’s disease. Molecular neurodegeneration. 2011;6(1):69. FREE FULL-TEXT.
- Kaplan BJ, Giesbrecht G, Shannon S, McLeod K. Evaluating treatments in health care: the instability of a one-legged stool. BMC Med Res Methodol. 2011;11:65. FREE FULL-TEXT. Abstract includes: “The purpose of this paper is to raise questions about over-reliance on RCTs and to point out an additional perspective for evaluating healthcare evidence, as embodied in the Hill criteria….Excessive reliance on RCTs tends to stifle funding of other types of research, and publication of other forms of evidence. We call upon our research and clinical colleagues to consider additional methods of evaluating data, such as the Hill criteria. Over-reliance on RCTs is similar to resting all of health care evidence on a one-legged stool.”
- Hachinski V, Donnan GA, Gorelick PB, Hacke W, Cramer SC, Kaste M, et al. Stroke: working toward a prioritized world agenda. Stroke. 2010 Jun;41(6):1084-99. FREE FULL-TEXT. Quote: “It is time to step into other domains so that knowledge in other areas may be readily applied to the problem of stroke. In other words, we need to scan the scientific landscape to embrace new ideas and approaches.”
- McNaull BB, Todd S, McGuinness B, Passmore AP. Inflammation and anti-inflammatory strategies for Alzheimer’s disease–a mini-review. Gerontology. 2010;56(1):3-14. FREE FULL-TEXT. Article includes: “In particular, the recent trial with etanrcept [citing to Tobinick, E.L. and H. Gross, Rapid cognitive improvement in Alzheimer’s disease following PSE administration. J Neuroinflammation, 2008. 5: p. 2] has provided much insight into pathogenesis and possible future treatment options. Not only does this anti-inflammatory agent improve results of memory testing (MMSE) over a 6-month period, it also has been shown to improve verbal fluency and apraxia in patients. Etanrcept is a specific antagonist of TNF-alpha. Studies now suggest that TNF-alpha may also regulate synaptic transmission and mediate beta-amyloid and beta-amyloid oligomer disruption of memory mechanisms. The rapid onset of effect with etanrcept suggests the synaptic effect is the most important.”
- Trollor, J.N., E. Smith, B.T. Baune, N.A. Kochan, L. Campbell, K. Samaras, J. Crawford, H. Brodaty, and P. Sachdev, Systemic inflammation is associated with MCI and its subtypes: the Sydney Memory and Aging Study. Dement Geriatr Cogn Disord, 2010. 30(6): p. 569-78. FREE FULL-TEXT.
- Ward, A.C., The role of causal criteria in causal inferences: Bradford Hill’s “aspects of association”. Epidemiol Perspect Innov, 2009. 6: p. 2. FREE FULL-TEXT.
- Reynolds, C.F., 3rd, D.A. Lewis, T. Detre, A.F. Schatzberg, and D.J. Kupfer, The future of psychiatry as clinical neuroscience. Acad Med, 2009. 84(4): p. 446-50. FREE FULL-TEXT. Abstract includes: “…advances in assessment, treatment, and prevention of brain disorders are likely to originate from studies of etiology and pathophysiology based in clinical and translational neuroscience.”
- McAlpine FE, Lee JK, Harms AS, Ruhn KA, Blurton-Jones M, Hong J, et al. Inhibition of soluble TNF signaling in a mouse model of Alzheimer’s disease prevents pre-plaque amyloid-associated neuropathology. Neurobiol Dis. 2009 Apr;34(1):163-77. FREE FULL-TEXT.
- Howick J, Glasziou P, Aronson JK. The evolution of evidence hierarchies: what can Bradford Hill’s ‘guidelines for causation’ contribute? J R Soc Med. 2009 May;102(5):186-94. FREE FULL-TEXT. Quote: “Evidence–grading systems that place randomized trials at the top of a hierarchy will deliver misleading conclusions in cases where RCTs are insufficient or unnecessary.”
- Holmes C, Cunningham C, Zotova E, Woolford J, Dean C, Kerr S, et al. Systemic inflammation and disease progression in Alzheimer disease. Neurology. 2009 Sep 8;73(10):768-74. FREE FULL-TEXT.
- Kaushal, V. and L.C. Schlichter, Mechanisms of microglia-mediated neurotoxicity in a new model of the stroke penumbra. J Neurosci, 2008. 28(9): p. 2221-30. FREE FULL-TEXT. Abstract concludes: “Together, these results support potential therapeutic strategies that target microglial group II mGluRs, TNFalpha overproduction, and NF-kappaB activation to reduce neuron death in the ischemic penumbra.”
- Wolinsky H. Paths to acceptance. The advancement of scientific knowledge is an uphill struggle against ‘accepted wisdom’. EMBO Rep. 2008 May;9(5):416-8. FREE FULL-TEXT. Article includes: “Unfortunately, scientists do not always follow a path of pure logic, as the German physicist Max Planck (1858–1947) once observed, “[a] new scientific truth does not triumph by convincing its opponents and making them see the light, but rather because its opponents eventually die, and a new generation grows up that is familiar with it.” The history of science is replete with theories that only became accepted by the scientific community after a long and protracted uphill battle.”
- Griffin WS. PSE: potential as an Alzheimer therapeutic. J Neuroinflammation. 2008;5:3. FREE FULL-TEXT.
- Glasziou P, Chalmers I, Rawlins M, McCulloch P. When are randomised trials unnecessary? Picking signal from noise. BMJ. 2007 Feb 17;334(7589):349-51. FREE FULL-TEXT. Quote: “The relation between a treatment and its effect is sometimes so dramatic that bias can be ruled out as an explanation.”
- Aronson, J.K. and M. Hauben, Anecdotes that provide definitive evidence. BMJ, 2006. 333(7581): p. 1267-9. FREE FULL-TEXT.
- Vandenbroucke, J.P., In defense of case reports and case series. Ann Intern Med, 2001. 134(4): p. 330-4. ABSTRACT.
- Hrobjartsson, A. and P.C. Gotzsche, Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med, 2001. 344(21): p. 1594-602. FREE FULL-TEXT. Abstract includes: “We found little evidence in general that placebos had powerful clinical effects.”
- McDonald, C.J., Is the placebo powerless? N Engl J Med, 2001. 345(17): p. 1276-7; author reply 1278-9. FREE FULL-TEXT. Authors’ reply includes: “The interesting commentaries did not demonstrate flaws in our systematic review, so our conclusion that there is little evidence that placebo interventions in general have powerful effects remains unchanged…..the burden of proof now rests with those who claim there are important effects of placebo interventions. Such claims should be based on reliable evidence, preferably data from rigorously conducted, systematic reviews of randomized trials.“
- Vandenbroucke, J.P., Case reports in an evidence-based world. J R Soc Med, 1999. 92(4): p. 159-63. FREE FULL-TEXT. Quote: “For true intellectual advancement, i.e. in proposing new problems, new solutions, or new ideas, the hierarchy is of necessity reversed. Solidly on top sits the case report and case series – observations of first cases, of mechanisms, of etiological or therapeutic surprises.”
- ***Horowitz, S.H., Thrombolytic therapy in acute stroke: neurologists, get off your hands! Arch Neurol, 1998. 55(2): p. 155-7. FULL-TEXT. Discussing the use of TPA as a treatment for acute stroke, the article discusses the resistance of the neurological community: “I am writing to convey my impressions of the lack of enthusiasm for this therapy [TPA for acute stroke] exhibited by neurologists at places where I have spoken. Rather than embrace, or at least acknowledge, this as the first step in the treatment of neurology’s most common serious and debilitating disease (Alzheimer disease excepted), it often has been met with skepticism, criticism and denial, with discussions centered around why t-PA cannot or should not be used, rather than how it could be used. Such negativism is now evident in the neurological literature in an article with the unambiguous title: “Tissue-type Plasminogen Activator Should Not Be Used in Acute Ischemic Stroke” ” Horowitz 1998 ***Of significant historical relevance
- Sackett, D.L., W.M. Rosenberg, J.A. Gray, R.B. Haynes, and W.S. Richardson, Evidence based medicine: what it is and what it isn’t. BMJ, 1996. 312(7023): p. 71-2. FREE FULL-TEXT. Quote: “Evidence based medicine is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based medicine means integrating individual clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise we mean the proficiency and judgment that individual clinicians acquire through clinical experience and clinical practice. Increased expertise is reflected in many ways, but especially in more effective and efficient diagnosis and in the more thoughtful identification and compassionate use of individual patients’ predicaments, rights, and preferences in making clinical decisions about their care. By best available external clinical evidence we mean clinically relevant research, often from the basic sciences of medicine, but especially from patient centered clinical research into the accuracy and precision of diagnostic tests (including the clinical examination), the power of prognostic markers, and the efficacy and safety of therapeutic, rehabilitative, and preventive regimens. External clinical evidence both invalidates previously accepted diagnostic tests and treatments and replaces them with new ones that are more powerful, more accurate, more efficacious, and safer.”
- Batson OV. The Function of the Vertebral Veins and Their Role in the Spread of Metastases. Ann Surg. 1940 Jul;112(1):138-49. FREE FULL-TEXT.
Figure 4, from Poon VY, Choi S, Park M. Growth factors in synaptic function. Front Synaptic Neurosci. 2013;5:6, used in accordance with its Creative Commons Attribution License (CCBY):